A new medical device to monitor a patient’s air flow
Guelay Bilen-Rosas has been an anesthesiologist for two decades, and she has participated in tens of thousands of surgeries. A big part of her job is to monitor vital signs and keep patients alive during surgery and afterward.
More and more, Bilen-Rosas has grown frustrated with the lack of equipment to keep an eye on a patient’s air flow post-surgery. “What blood is for heart, air flow is for the lungs,” she says. “During surgery, a breathing tube is connected to a ventilator with a sensor that provides all the data in the world. But after surgery, the tube comes out and we lose all of that data.”
As a result, medical personnel have no definitive way to gauge a patient’s respiration post-surgery. Even a pulse oximeter, which measures the oxygen content in red blood cells, doesn’t immediately reveal a decline. If a problem exists, there’s no way to identify it until the patient is past the safety threshold and heading into respiratory failure.
 That gap has deeply troubled Bilen-Rosas. “As an anesthesiologist, I give my patients, in their most vulnerable state, to nurses who have practically no data to monitor air flow. There are a lot of near misses. That is not acceptable. I’m ashamed that we cannot do better,” she says.
That gap has deeply troubled Bilen-Rosas. “As an anesthesiologist, I give my patients, in their most vulnerable state, to nurses who have practically no data to monitor air flow. There are a lot of near misses. That is not acceptable. I’m ashamed that we cannot do better,” she says.
A small, wearable device
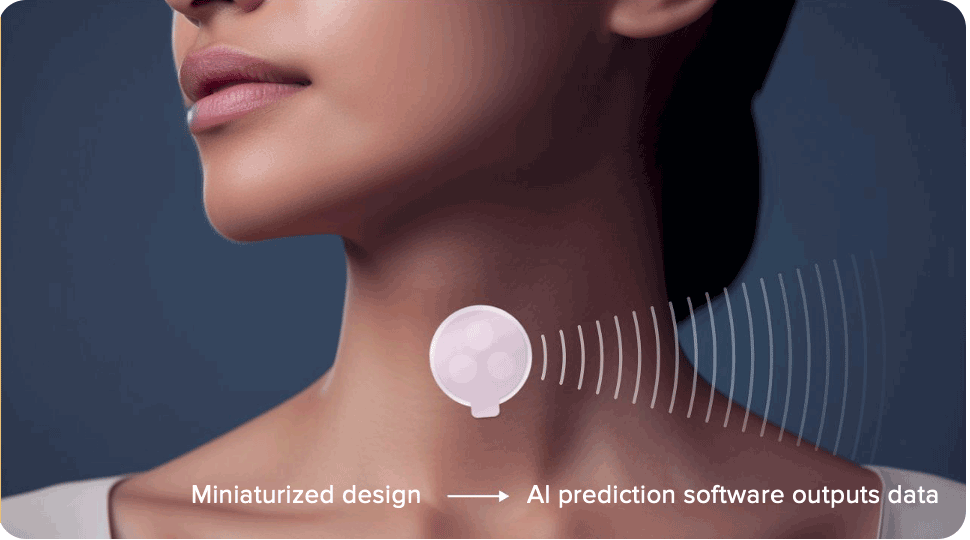
What AyrFlo Innovation Labs has developed is the SmartAYRpatch, a small patch—about the size of a nickel, initially—that sticks on the front of a patient’s throat. “We have been able to develop the first noninvasive, wearable, complete breathing monitor device that will close that data gap,” she says.
In the current design, the patch is wired to a laptop. Eventually, it will be smaller and will use an app that can send data into a smartphone or computer.
The technology is based on ultrasound waves. “Ultrasound is traditionally used for imaging—big machines that allow image-guided diagnostics. I don’t use the images; I am using the physics of ultrasound. When it travels through tissue, it gives an altered wave, and that gives us information about the body’s operation,” Bilen-Rosas says. “It is the most comprehensive breathing data so that we can begin intervening and helping our patients who need support to prevent respiratory complications.”
Bilen-Rosas was born in Istanbul; her family moved from Turkey to Germany when she was four years old. Her beginnings were “very humble,” she says. Her mother cleaned the local hospital and her father worked in a factory. “But we had love; we had hope. I was raised by the two wisest human beings that I know.” Bilen-Rosas earned a medical degree from Johannes Gutenberg University in Mainz, Germany, and completed a residency at Barnes Jewish Hospital, part of Washington University in St. Louis, and a fellowship at St. Louis Children’s Hospital.

Dr. Guelay Bilen-Rosas and Dr. Humberto Rosas
In addition to her clinical work, as an associate professor in anesthesiology at UW-Madison, Bilen-Rosas’s lab started working on the technology in 2015; within one year, she obtained her first patent. Bilen-Rosas and her husband, UW radiologist and professor Humberto Rosas, cofounded AyrFlo in 2020. “He said early on, ‘I will support your dream.’ Without his support, I would not have been able to do this.”
Raising funds has been a challenge, Bilen-Rosas says. “The business of entrepreneurship takes time. The battle is tough for anybody. It’s really hard for first-time founders—especially if they are women.” According to PitchBook, businesses founded by women received only 2% of the venture capital investments in 2022 and 2023.
Accumulating patents and investors
Today, AyrFlo is housed in Forward BIOLABS in Madison and has a staff of six. The Wisconsin Alumni Research Foundation (WARF) has been one of Bilen-Rosas’s staunch supporters. AyrFlo won a $10,000 WARF Innovation Award and has received additional funding from the WARF Accelerator program.
 Through WARF, AyrFlo has licensed seven patent applications and has five issued patents in the U.S. and internationally. “We are excited about the opportunity her technology provides to fundamentally change the way patients are monitored under sedation. We have supported her efforts, in her dual role as a physician and entrepreneur, to translate her research into societal impact through a startup,” says Greg Keenan, senior director of WARF Accelerator and WARF Ventures.
Through WARF, AyrFlo has licensed seven patent applications and has five issued patents in the U.S. and internationally. “We are excited about the opportunity her technology provides to fundamentally change the way patients are monitored under sedation. We have supported her efforts, in her dual role as a physician and entrepreneur, to translate her research into societal impact through a startup,” says Greg Keenan, senior director of WARF Accelerator and WARF Ventures.
AyrFlo also received a $12,500 We’re All In Innovating Grant from WEDC in 2020 and is certified by WEDC as a Qualified New Business Venture, allowing the company’s investors to receive state tax credits.
To date, AyrFlo has raised $800,000 from angel investors around the country. Bilen-Rosas hopes the next funding round will help finance the first working prototype of the SmartAYRpatch, which will have to go through clinical trials to win approval from the U.S. Food and Drug Administration. Bilen-Rosas hopes the patch will be available for use in three years. Eventually, it could be used to track breathing in any situation, from hospital to home health care, including people with asthma, athletes in training, or soldiers wounded in combat, Bilen-Rosas says.
Developing a medical device and founding a company is risky, she says, but worth the effort. “You have to stay true to what your dreams are. Never doubt yourself. Surround yourself with people who believe in the impossible,” Bilen-Rosas says.